Providers Guide to Setup Remote Patient Monitoring and Maximize Reimbursement
The healthcare system in US is moving towards value-based care, where providers are rewarded for delivering better outcomes, that prevents complications, and reduces costs. With the increase in aging population, rising chronic diseases Remote Patient Monitoring is shifting care from a reactive, episodic model to a proactive, continuous one. By using FDA-approved devices they monitor patients securely from the comfort of their home. In this blog let us see how a phased and strategic planning helps providers to setup RPM that results in better patient outcomes, optimized reimbursements, and a scalable care delivery system.
How does Remote Patient Monitoring helps Providers?
Remote patient monitoring (RPM) allows providers to extend their services beyond the premises of their clinic. They help to track and monitor chronic conditions like diabetes, hypertension, COPD, and heart failure through connected medical devices improving patient outcomes while unlocking a new stream of revenue. With CMS expanding the coverage for remote patient monitoring, it has also become a financial tool for providers giving them a new opportunity to bill Medicare and private insurers for ongoing care management, increasing patient engagement while ensuring financial sustainability.
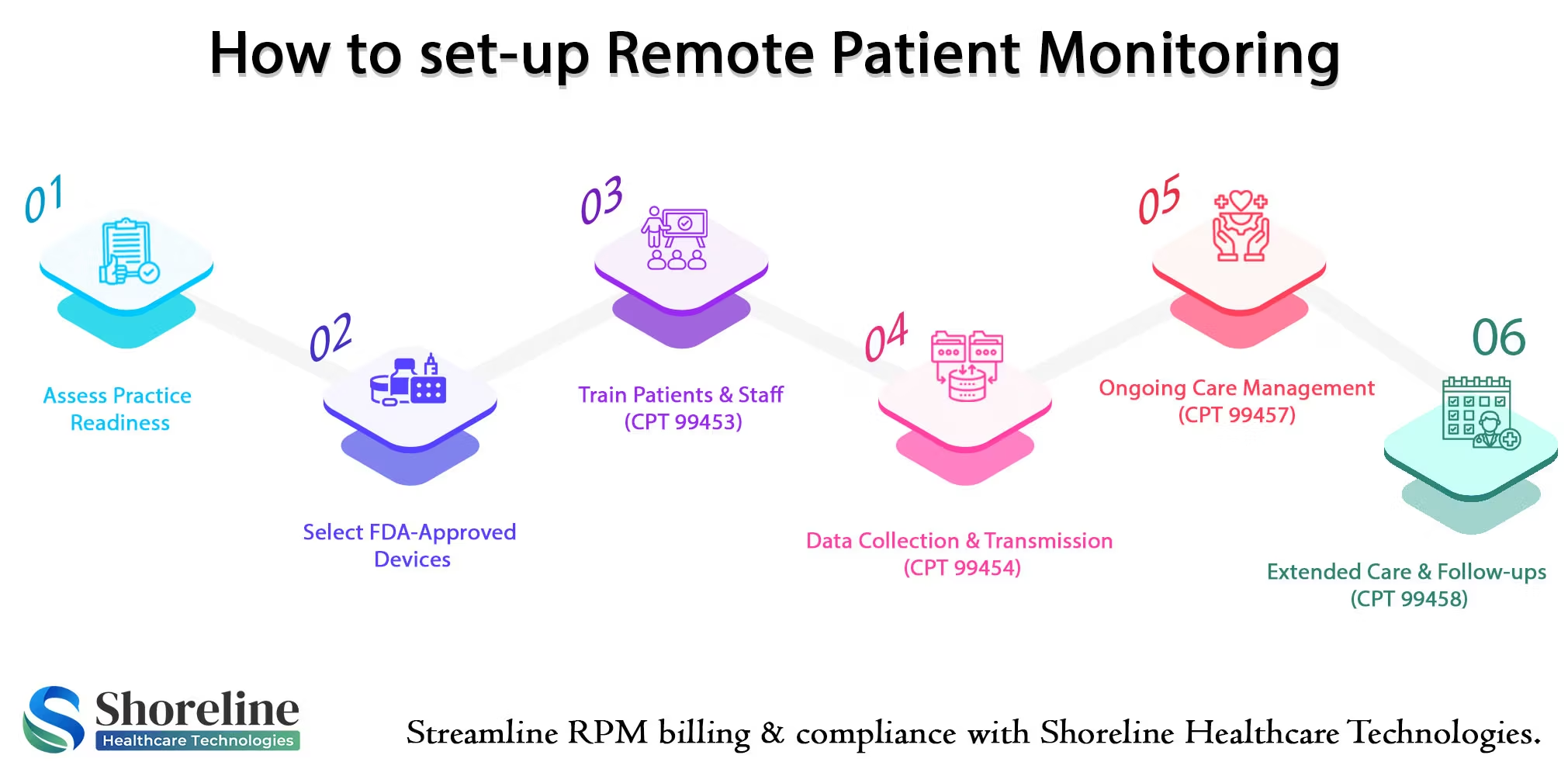
Setting Up the RPM Program
Setting up a remote patient monitoring (RPM) program needs careful planning and training for staffs and patients. It should be an effective, human-centered system with ongoing evaluation.
Readiness and Strategic Planning
Before adopting an RPM platform organization must conduct a thorough readiness assessment.
- Organizational Viability: Assess whether implementing RPM platform is clinically viable and technically feasible, for the organization considering their specific patient population.
- Program Goals: Define clear, distinct goals for the program. Different patient conditions or target populations will have different clinical, cost, and operational needs.
- Identify the eligible Patients: Choose people who benefits from remote monitoring like patients with chronic conditions, those recovering from surgery or who are most likely to engage with the technology. As per CMS guidelines patients with chronic conditions are more likely to get reimbursements. Choosing the eligible patients help to have an effective program and maintain long-term sustainability.
Building the Right Team
Implementing any successful program requires a dedicated team with complete knowledge for handling the new work task.
- Appoint a Team with Multidisciplinary personnel like physicians, nurses, clinical staffs, IT specialists, and quality assurance experts for setting up the program and managing the data.
- Pick up the Right Partner who can provide a complete solution like integrating with existing electronic health records (EHRs), procuring the medical device, handling logistics, and educating the patients. So that the complexities of hiring and managing new IT infrastructure is reduced.
Essential System Architecture
An effective RPM system, requires a multi-layered ecosystem built with robust technological infrastructure and core components like a secure cloud environment, real-time data analytics, and data management tools to handle the large volume of patient information. They must easily integrate and interoperable with all systems. Choose FDA approved Medical Devices that can securely collect and transmit health data in real-time.
Providing Staff Training and Patient Education
Train the staffs on how the RPM system work and give them clear roles and responsibilities like monitoring data, managing alerts, and communicating with patients. Providing a clear, standardized procedures help to have an efficient workflow.
Educate Patients on how to use their devices and make them understand their role in the monitoring process. Enlighten them with the CMS guidelines and requirements for taking measurements consistently for at least 16 days a month, for getting reimbursement.
Obtaining and Documenting Patient Consent
Before starting the monitoring process get consent from patients. It can be verbal or written but must be documented in the patient's medical record. It should be obtained by the billing practitioner before services are rendered and inform them about their co-pays or deductibles.
Managing the Data and Monitoring the outcome
Quicker clinical interventions and effective data management are the key factors for the success of RPM programs. To achieve this provider can set emergency alerts for any fluctuations in readings and appoint a dedicated team for escalating issues to the appropriate care team.
Continuous Improvement
Conduct periodic reviews and audits to check the program's success and identify inefficiencies so that it can be scaled up to a broader patient population over time.
By partnering with Shoreline Healthcare Technologies providers can effectively setup their remote patient monitoring setup and get higher revenues with a phased approach. Thereby making healthcare more efficient, patient-centered, and financially viable care model.
Shoreline Healthcare Technologies: Your RPM Billing Partner
We at Shoreline Healthcare Technologies specialize in remote patient monitoring billing. Our service includes device setup documentation and assigning correct CPT codes. We help providers with virtual assistants to enroll patients efficiently, document and track the RPM data for billing, stay in compliant with Medicare telehealth reimbursement requirements. Our expert team reduces denials and helps to get maximum reimbursement for all your services.
FAQs
Q1. How many days of data are required for RPM reimbursement?
+At least 16 days of patient data are required as per CMS guidelines for a 30-day billing cycle to get reimbursements for RPM.
Q2. Does Medicare cover remote patient monitoring services?
+Yes. Medicare do cover RPM services. Providers must use medical devices approved by FDA and bill with correct CPT codes that meets the CMS Standards.
Q3. Is RPM the same as telehealth?
+No. Telehealth involves live virtual calls or videos, whereas RPM monitors and collects the patient’s vitals in real-time secure medical devices.
Q4. Are RPM services reimbursed by private insurers?
+Yes. Many commercial payers follow CMS guidelines for reimbursement however the rate and other policy terms vary by payer, contract terms, and state regulations.
Q5. Can RPM be billed for acute conditions?
+While RPM is primarily used for chronic conditions, it may also be billed for acute conditions when medically necessary and properly documented.
Q6. How can Shoreline Healthcare Technologies help with RPM reimbursement?
+We at Shoreline Healthcare Technologies simplifies RPM billing with expert coding, compliance checks, and revenue cycle management, for getting maximum reimbursement.
Q7. Is ShorelineMB the same as Shoreline Healthcare Technologies?
+Yes, ShorelineMB.com is the official website of Shoreline Healthcare Technologies, a leading provider of medical billing and RCM services.


















Contact Shoreline Healthcare Technologies today for a personalized demo.