|
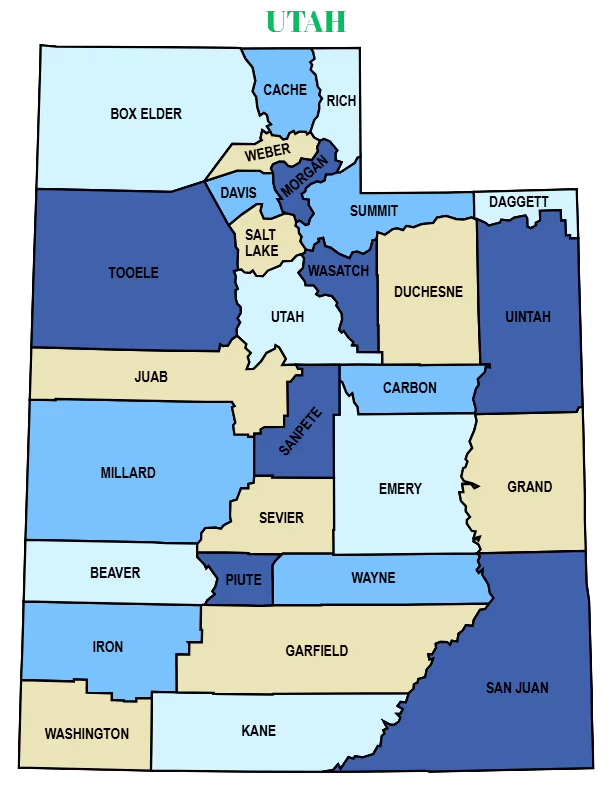
Utah Medicaid & MCO Claims Processing
|
Claims routed accurately based on Fee-for-Service, ACO, managed care, and waiver eligibility with Utah-specific billing logic
|
25–40% reduction in denial rates with faster reimbursement cycles.
|
Claims submitted within 24–48 hours
|
|
Eligibility Verification & Monitoring
|
Real-time eligibility checks aligned with Utah’s retroactive eligibility rules, ACO attribution models, and managed care enrollment changes
|
Reduction in eligibility-related denials by 30–45%
|
Instant/ Within 24 hours
|
|
Prior Authorization Management
|
End-to-end tracking of service-specific, provider-specific, and time-bound authorizations required under Utah Medicaid
|
40–60% reduction in PA-related denials
|
3–5 business days
|
|
Provider Enrollment & Revalidation
|
Utah Medicaid enrollment, revalidation, and MCO credentialing, aligned with current state workflows
|
Eliminates enrollment related denials.
|
3-4 weeks
|
|
Behavioral & Physical Health Billing Support
|
Correct routing of behavioral and physical health claims to prevent cross-program denials
|
Improved reimbursement for integrated care visits
|
24–72 hours
|
|
Timely Filing Management
|
Monitoring of Utah Medicaid and MCO-specific filing limits to prevent revenue loss
|
Significant reduction in late-filing write-offs
|
Ongoing, automated
|
|
Denial Management
|
AI based tools to track and flag denial codes and root-cause analysis tailored for Medicaid claim categories, identifies high-risk categories and automate resubmissions.
|
Reduce rate of denial by 75% and with quicker appeals.
|
7–14 days for backlog cleanup; ongoing daily follow-up
|
|
Patient Statements & Follow-Up
|
Communicate with patients and give Explanation of Benefits (EOBs). Includes text/email payment reminders and online payment options.
|
Reduces overdue balances and increases the collection rates.
|
1-2 weeks
|
|
Audit & Compliance Support
|
Conducts Audit Review and mock audits, including documentation, encounter verification, and claim reconciliation.
|
Minimizes risk of penalties and supports successful audits.
|
Ongoing, depending on audit schedule
|










.png)
