
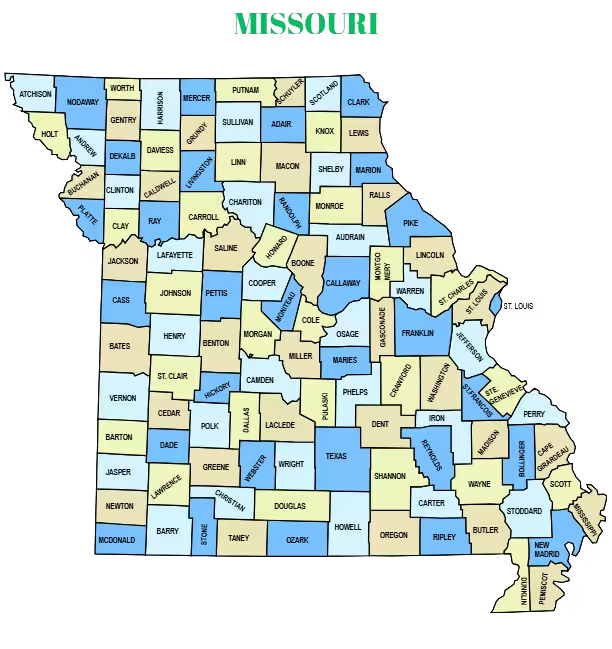
Shoreline Healthcare Technologies is a proud Maine-based company that offers end to end revenue cycle management services to physicians and Medical billing companies in Missouri. Our goal is to help them manage their business in a way where they can focus on patient care and operations, not paperwork! By providing great services at reduced costs, we have been able to keep our customers since our inception in 2015. Explore our case studies to see how we’ve helped practices overcome complex billing challenges and improve cash flow.
As a medical billing outsourcing company, we have helped our clients grow their business by providing them with the resources they need to succeed while maintaining a competitive edge in today’s industry. We offer timesaving, cost-effective revenue cycle management services to your Missouri-based practice. Ready to outsource your billing needs? We’ll guide you through your receivable account to make sure that your claims are paid.











.png)
