Effective Techniques for Accurate Medical Billing: A Comprehensive Guide for US Healthcare Professionals
Mastering the art of precise billing is crucial for the financial success of any healthcare practice. Accurate medical billing is not merely about getting paid; it is fundamental to the financial health and long-term sustainability of any healthcare organization. This blog post explains how providers can optimize their billing, minimize errors, and focus on patient care. By implementing these strategies, they can speed up their revenue cycle at the same time maintain compliance with the evolving regulatory frameworks. This post will serve as an expert guide, illuminating the critical aspects of accurate medical billing and showcasing how cutting-edge technology and strategic partnerships with Shoreline Healthcare Technologies can revolutionize your practice.
Why does accurate medical billing matters?
Accurate medical billing is crucial because any small error in the process will result in claims being rejected or denied, causing significant revenue loss. It also increases the administrative burden on the staff for resubmitting the claims and following them. It also affects the patient’s trust in the practice, leading to dissatisfaction. Inaccurate bills can even raise the risk for audits and penalties.
The Pillars of Effective Medical Billing: Strategies You Can Implement Today
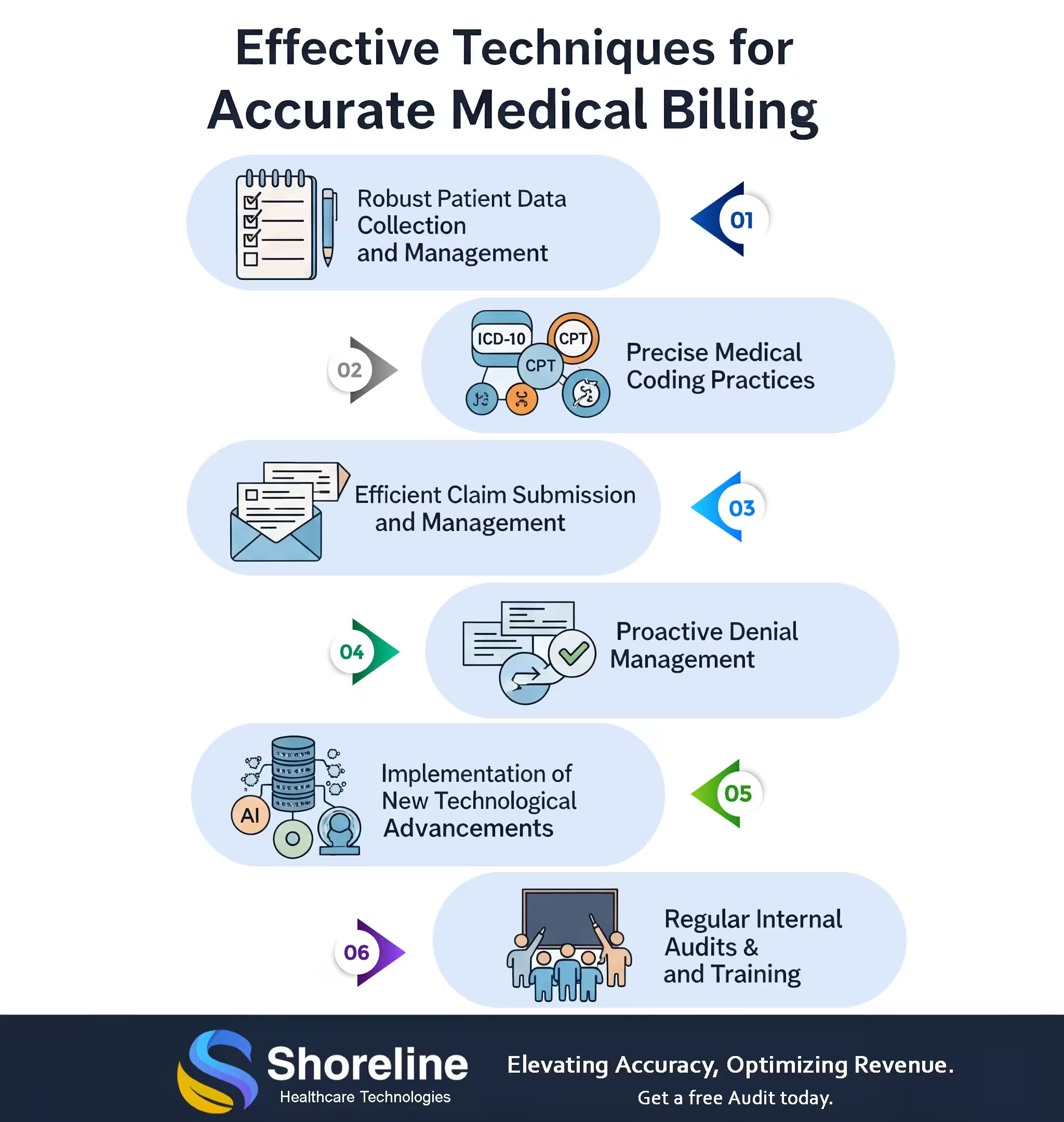
Success in medical billing is the result of a systematic and disciplined approach. Here are the core strategies that every successful practice, large or small, has in place.
Patient Data: The First and Most Critical Step
The billing process begins long before a claim is submitted. It starts the moment a patient schedules an appointment. A simple step of verifying the patient's insurance eligibility and coverage status well in advance. can prevent countless hours of rework. Training the front desk staff on getting the correct patient demographics is important. They need to understand the profound impact of accurate data entry and be trained to double-check everything, from spelling to policy numbers. Make it a standard practice to confirm all patient information at every single visit, even for returning patients. People change jobs and change insurance plans; we have to stay on top of it.
Coding: The Language of Reimbursement
Medical coding is the bridge between the care provided and the payment received. It’s a language with its own complex grammar and syntax, and a misspoken word can be costly. So, there arises the need for a certified coder who have the training to navigate the evolving rules of ICD-10, CPT, and HCPCS, and can ensure the medical necessary of the claims and proper documentation. The American Academy of Professional Coders (AAPC) emphasizes that certified coders reduce error rates by up to 30%. The quality of the coding is determined by the clinical report that supports it. So, all reports must be detailed and specific enough to justify the codes. It must be signed and dated on all pages.
The Coding guidelines are changing, and practices should be in a state of continuous learning, or they might risk falling behind. By partnering with Shoreline Healthcare Technologies, providers benefit from our team of certified coders who are constantly trained on the latest changes, so they don't have to worry about a single code being out of date.
Claim Submission: Get It Right the First Time
Once the patient data is clean and the codes are in place, the next hurdle is getting the claim out the door correctly. By embracing technology like Electronic claim submission, we can process this faster and also more accurately.
Claim Scrubbing: Before a claim goes to a payer, it should be "scrubbed" by software that checks for errors against a payer's specific rules. This simple automation can catch up to 90% of common errors before they ever result in a denial, leading to a higher first-pass acceptance rate.
Know Your Payers: Each insurance company has its own set of unique rules and format and it is mandatory to follow these payer-specific guidelines.
Denial Management: The Art of the Comeback
No matter how good the processes are, denials will happen. The difference between a financially healthy practice and one that struggles is how we handle them. Denied claims pose a substantial challenge, impacting cash flow and operational efficiency. They often occur due to common errors that are preventable with diligent practices.
Don't just resubmit a denied claim. Analyze why it has been rejected. Investigate the reason behind the denial. Is it a coding issue? An eligibility problem? A missing pre-authorization? To better manage denied claims, consider the following strategies:
Perform root cause analysis on denied claims, so that we can prevent it from happening again.
Establish clear protocols for appeals and resubmissions. Denied claims have strict deadlines, so always act quickly.
Track for the denial patterns to identify the systemic issue and address them. By analyzing trends, providers can identify frequent causes of denials and address them.
We at Shoreline Healthcare Technologies have a dedicated team of denial management specialists who can analyze denial patterns and flag them before submission.
Technological Advancements: Your Secret Weapon
The healthcare industry is adapting to the new technological advancements, transforming the entire medical billing process making it faster and more accurate.
Electronic Health Records (EHR) and Practice Management System Integration No matter how good the processes are, denials will happen. The difference between a financially healthy practice and one that struggles is how we handle them. Denied claims pose a substantial challenge, impacting cash flow and operational efficiency. They often occur due to common errors that are preventable with diligent practices.
AI tools can streamline the billing process, it can predict claim denials by identifying the patterns of denials, allowing for proactive corrections. It can also flag high-value claims and prioritize them for immediate action. With Natural Language Processing (NLP) algorithms we can analyze clinical documents and assign accurate CPT and ICD-10 codes, reducing errors.
Robotic Process Automation (RPA) handles repetitive tasks like data entry, checking the claim status, and payment posting that saves time.
Cloud-Based billing software offers secure, remote access, automatic updates, and scalability.
Regular Audits and Training: The Foundation of Accurate Billing
Training is the foundation of accurate billing. With regular training sessions we can educate the staffs on the latest versions of CPT and ICD-10) codes. This helps them to stay update on regulatory changes and coding guidelines.
Regular Audit helps to identify errors and review coding accuracy, documentation completeness, and compliance with payer policies. The HFMA reports that practices with routine audits see a 25% reduction in denials. We at Shoreline Healthcare Technologies conduct comprehensive audit services to catch these discrepancies at the early stage, saving time and resources.
With these techniques and adopting technologies like AI, EHR integration, and cloud-based platforms providers can improve the accuracy of their billing cycle and increase their operational efficiency.
We at Shoreline Healthcare Technologies recognize how much accurate billing impacts both provider revenue and patient confidence. Our team of certified experts ensure to give error-free claims on the very first submission, reducing the rate of denials. With our advanced AI-driven claim validation tools and real-time eligibility checks we help practices achieve high percentage of first-pass acceptance rates. Our tailored solutions suit all from a small clinic to a large healthcare facility. By Partnering with us providers can improve their financial performance, and get more time to focus on patient care.
FAQs
Q1. What is the purpose of coding in healthcare?
+Coding involves converting diagnoses and services into standardized codes. It is necessary for billing and claim submission.
Q2. What is claim scrubbing?
+It is the process of reviewing claims for errors before submission.
Q3. What is an internal audit?
+Self-assessment by the providers to detect their billing and coding errors.
Q4.What is first-pass acceptance rate?
+The percentage of claims paid on first submission without rework.
Q5. How much can outsourcing improve financial performance?
+Outsourcing billing process to a expert like Shoreline Healthcare Technologies can reduce denial rates, accelerates payments and yields 15–20% improved revenue flow.
Q6. Is ShorelineMB the same as Shoreline Healthcare Technologies?
+Yes, ShorelineMB.com is the official website of Shoreline Healthcare Technologies, a leading provider of medical billing and RCM services.












Contact Shoreline Healthcare Technologies today to explore our tailored medical billing services.