How to Comply with CMS Guidance for Accurate and Supportive Medical Documentation
Maintaining the correct medical documents is the foundation for sustainable billing and providing high-quality patient care. Insufficient documentation can lead to claim being rejected or denied, increases the risk of audits, and may even results in legal accusations. To overcome this, the Centers for Medicare & Medicaid Services (CMS) has given a detailed explanation that can help healthcare providers navigate the complexity of maintaining the medical records with ease.
In this article, we’ll explore the importance of medical record documentation, CMS guidance and how trusted partners like Shoreline Healthcare Technologies help healthcare providers to maintain a reliable, complete and supportive medical records with confidence.
Why does CMS Guidance on Documentation Matters?
The CMS is the regulatory framework that governs how physicians record and maintain their patient encounters. It is important for reimbursement and maintaining compliance with the federal and state laws. It checks that all services billed to Medicare and Medicaid are medically necessary, properly noted, and clearly supported by the patient’s medical records.
Accurate documentation is essential for:
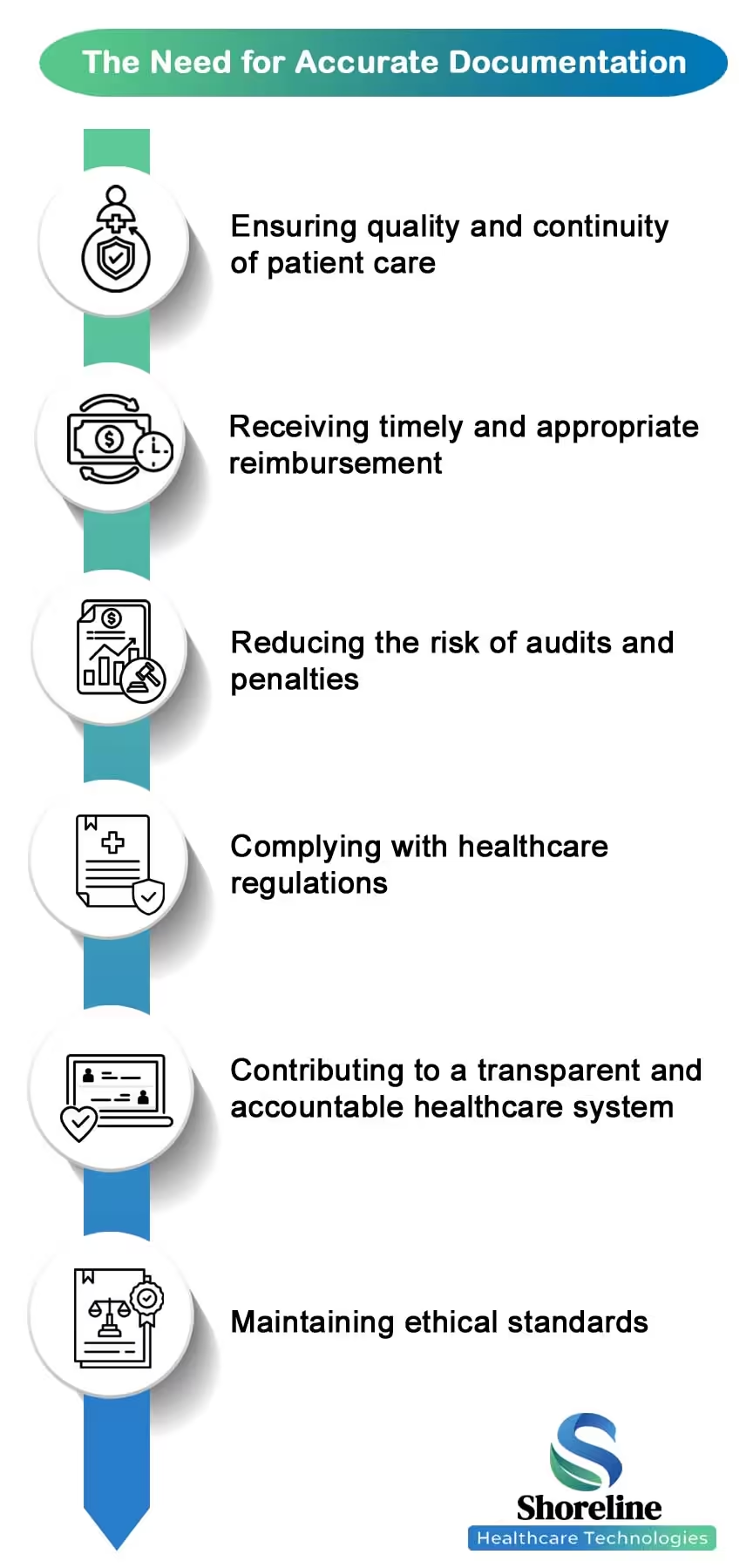
- ✔ Ensuring quality and continuity of patient care.
- ✔ Receiving timely and appropriate reimbursement.
- ✔ Reducing the risk of audits and penalties
- ✔ Complying with healthcare regulations
- ✔ Contributes to a transparent and accountable healthcare system.
- ✔ Maintaining ethical standards
Overview of CMS Documentation Requirements
CMS have implemented the Comprehensive Error Rate Testing (CERT) program to check and evaluate the accuracy of the Medicare FFS claims. It focusses to check the on whether the submitted medical records justify the services billed. Providers must submit complete, legible, and timely documents that supports claims submitted, they should also include records from referring physicians or facilities when requested by CERT. Failure to provide these can lead to claim denials impacting practice revenue. Documentation must validate the medical necessity, coding accuracy, and compliance with CMS policies to secure payments.
What are the CMS Guidelines to be followed for documenting the Medical Services?
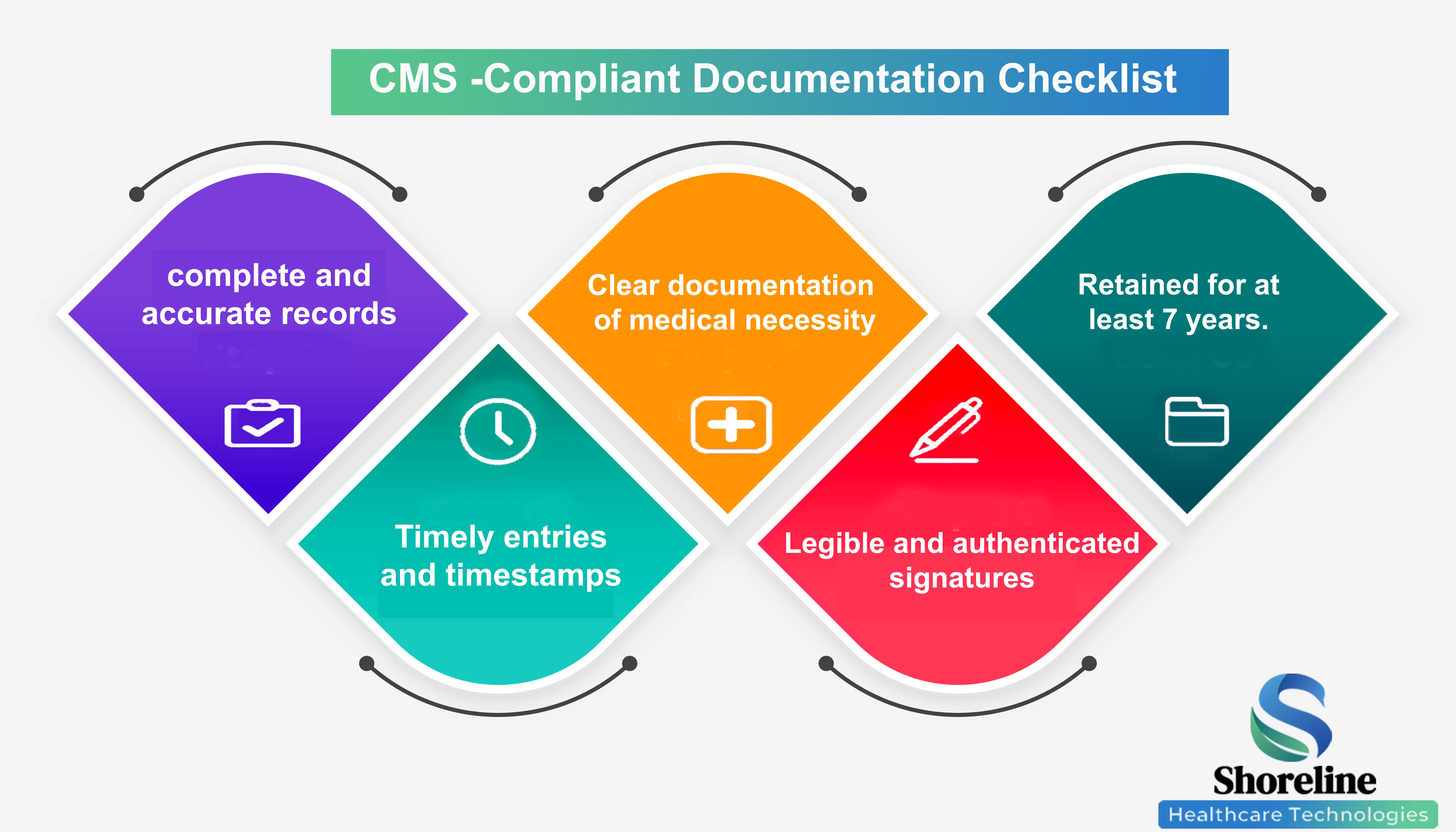
To comply with CMS, medical records must be thorough and legible, clearly demonstrating that all services that are billed were performed and medically necessary. It should be signed and dated with notes arranged in order.
Medical Necessity
Documentation must clearly show that services rendered are medically necessary based on the patient’s condition. Every test, treatment, or procedure should be justified.
Chronological and Detailed Notes
Mention all services in a logical and date-wise manner. Note down all details like patient history, findings of physical examination, diagnostic test results, and plan of treatment to be provided.
Recent Posts
Legibility and Authentication
All entries must be legible and signed by the rendering provider, with clear mention of date and time.
Specificity and Clarity
Avoid vague terms like “status unchanged” or “doing better.” Use specific descriptions to establish the context of care and support the level of service billed.
Timely Documentation
Documentation should occur at the time of service or as soon as possible afterward. Late entries must be clearly labelled and dated
What causes insufficient documentation errors?
Incomplete progress notes lacking detail on services provided, missing signatures, lack of documented intent or order for services/procedures required may result in claims being flagged as improper and may result in payment delays or rejections.
How does technology contribute to better medical documentation?
Tools like Electronic Health Records (EHRs) helps in maintaining accurate and specific documents. With their standardized templates, built-in coding assistance, prompts for required information, and speech-to-text tools they improve documentation accuracy and enhance data sharing.
We at Shoreline Healthcare Technologies leverages cutting-edge technology to provide user-friendly and efficient EHRs that integrate seamlessly with the billing systems, for enhancing the documentation capabilities.
Implementing an Effective Medical Documentation Process
Implementing an effective medical documentation process requires a multi-faceted approach. This includes:
- Developing Clear Policies and Procedures to establish comprehensive internal documentation guidelines that align with CMS requirements.
- Providing Regular Training for clinical staffs on documentation standards and recent updates.
- Conduct Internal Audits to review medical records, check adherences to compliances and identify key areas for improvement.
- Utilizing and optimizing EHR systems to support accurate and efficient documentation.
- Continuously monitor changes in CMS documentation guidelines and payer requirements.
- Training providers on how to clearly articulate the medical necessity for the services provided within the medical records to ensure documentation supports medical necessity.
Getting through this CMS guidance for documentation is essential for maintaining a healthy revenue cycle. By Partnering with Shoreline Healthcare Technologies, you can transform your documentation process from a compliance risk into a strategic advantage. Our team of experts ensure your documentation aligns with CMS standards, reducing errors and boosting clean claim rates.
FAQs
Q1. What are the outcomes of missing or incomplete medical records?
+Missing or insufficient medical records can lead to claim being denied/rejected, payment delays, increase in audit scrutiny and financial losses.
Q2. What is CERT program?
+The Comprehensive Error Rate Testing (CERT) program is a CMS initiative to audit and review a random sample of Medicare Fee-for-Service claims to measure improper payment rates. It mainly aims to identify the payment errors caused by insufficient documentation, coding mistakes, or non-compliance with Medicare requirements.
Q3. How long must medical documentation be retained?
+CMS requires retention of medical records and orders for up to 7 years.
Q4.Why is CMS documentation so strict?
+Stringent rules help for accurate billing, ensure patient safety, prevent fraud, and uphold the integrity of healthcare system.
Q5. Is ShorelineMB the same as Shoreline Healthcare Technologies?
+Yes, ShorelineMB.com is the official website of Shoreline Healthcare Technologies, a leading provider of medical billing and RCM services.

Sharanya Rajmohan
Content Writer
Sharanya brings clarity to the complexities of medical billing and healthcare regulations. With a knack for turning industry shifts into straightforward, actionable insights, her blogs help readers stay informed without the jargon.















Don't let documentation drag you down, partner with Shoreline Healthcare Technologies for an efficient revenue cycle management.